Issue #24: Does Your Job Require You to Provide Support or Accountability?
Both support and accountability are required to drive results, so understanding your role in this respect is critically important.
Support includes activities like education, 1:1 time, tools, communication, setting expectations, and other activities that help individuals achieve their goals. Accountability, on the other hand, facilitates individual responsibility including leveraging reports to ask tough questions, ensuring deadlines are met and that rules are enforced.
In the education field, our job is almost 100% support. What about yours?
Read More
Issue #23: Are You Checking it Twice? ...Your Staffing Grid, That Is!
Staffing grids connect clinical and financial guidelines in a way that effectively supports sustainable operations.
We aren't sure how long they've been around, but we would assume that the first staffing grid is older than anyone reading this, given how beautifully simple and impactful these little pieces of paper can be.
Does your nursing unit's staffing grid align with the budget financially? Are your nursing units staffing in alignment with their grids? How do you know? How do you ensure consistent nursing ratios between units? Across multiple hospitals in a health system?
Read More
Issue #22: Is your ER Full of Inpatients?!
Is the ER solely responsible for boarders at your hospital? If so, #youredoingitwrong!
While patients with admission orders waiting to go upstairs are physically in the ER, the drivers of their delay has very little to do with the ER itself. The truth about boarders is that they are primarily driven by inefficient processes on the inpatient side, while the ER pays the price.
Read More
Issue #21: Best Practices to Improve ER Throughput
According to the CDC, more than 1.5 million would-be ER patients leave without being seen each year in the US. Exacerbated by the pandemic, the Left Without Being Seen (LWBS) rate has skyrocketed, leading to significant lost revenue for hospitals who desperately need it to support staffing levels. Ensuring patients receive care when they need it is a critical part of supporting the communities we serve. Design a plan to keep both patients and finances healthy with proven ER best practices.
Read More
Issue #20: Is Your Float Pool Reliable?
Many organizations implement float pools to help cover unexpected gaps in schedules, but without a thoughtful approach and proper planning, they routinely fail – sometimes costing their organizations millions per month in avoidable spend with no end in sight.
Departments request float pool resources for all open shifts, regardless of the reason. However, successful labor leaders understand that each type of resource demand - due to vacancy, maternity leave, seasonal peak volumes, etc - requires a specific support strategy.
Read More
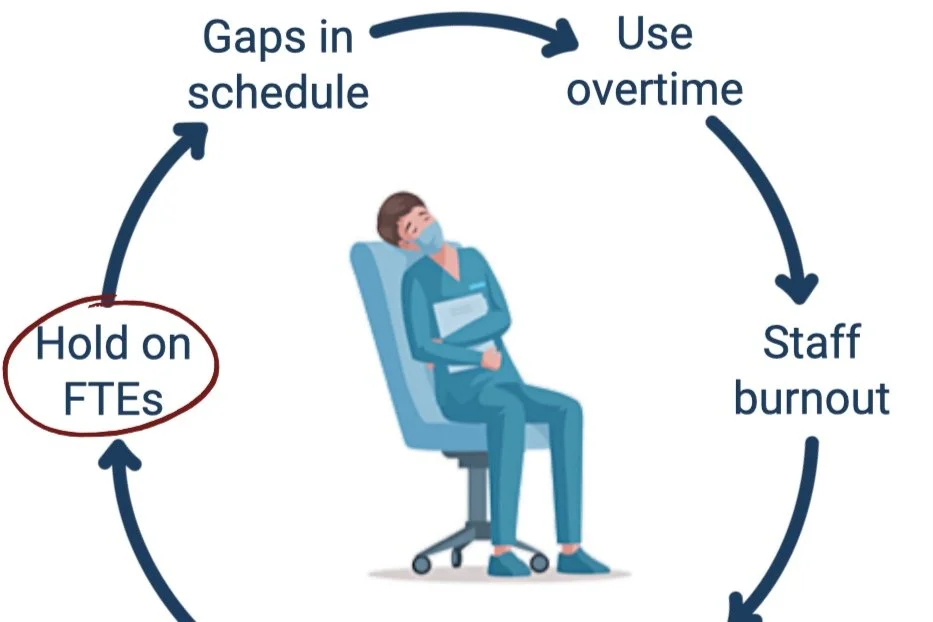
Issue #19: Perfecting Premium Pay: Hiring FTEs within the Goldilocks Zone
How does your hospital manage position approvals? We've observed 3 methods: Hiring to budgeted FTEs, approvals based on productivity performance, or customized department FTE hire targets based on total annual projected labor spend. Hire targets provide a specific FTE value for departments to maintain by considering volume-driven monthly FTE needs and total annual labor cost. For best results, start with the most cost effective option and make adjustments from there by carefully considering the operational feasibility of flexing up. Remember: the best way to address chronic vacancies is to hire ahead of turnover!
Read More
Issue #18: Common Sense Premium Pay Management Tactics
Hospitals define premium pay as any rate of pay above the base employed rate. Premium pay can include shift bonuses, weekend differentials, overtime, contract labor, and more.
Premium pay is of vital importance when staffing 24/7 patient care operations. By design, it acts as a financial incentive where needed to support balanced shifts and ensures we have the right staff, in the right place, at the right time, to provide optimal patient care.
Read More
Issue #17: Alternative Care Delivery Models
Nurse vacancies and contract labor rates have soared in the post-pandemic environment. As a result, many hospitals are currently evaluating alternative care delivery models to support the staffing ratios needed to provide quality patient care and retain staff. This newsletter reviews four alternative care delivery model options, ideas to attract applicants, and considerations for successfully implementing a change to your current care delivery model.
Read More
Issue #16: The Top 4 Drivers of Hospital Labor Budget Misses
While monthly performance tracking to budgeted goals is critical to the success of any business, hospitals tend to have more complex drivers of budget variance than other industries. Because workforce constitutes 50-60% of hospital spend and is widely considered the most controllable expense, labor is often the focus of budget variance conversations.
Read More
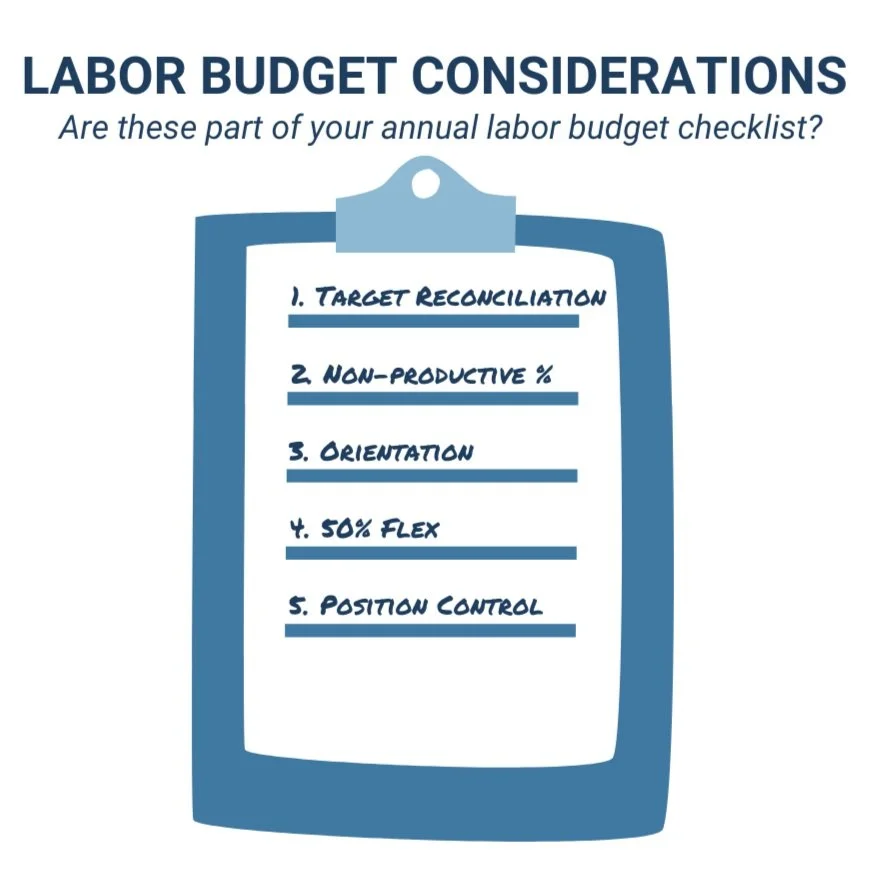
Issue #15: Annual Hospital Labor Budget Reminders
Department productivity drives hospital FTE performance to budget. High performing organizations proactively and thoughtfully cascade realistic FTE budgets to department productivity goals. After working with many hospitals and health systems over the years, our team has identified the top 5 labor budgeting practices that drive favorable FTE performance. These tactics significantly minimize budget risk by ensuring all risks can be mitigated through department action plans.
Read More
Issue #14: Don't Confuse Labor Benchmarks with Management Tools!
Labor benchmarks are commonly used in healthcare to inform leaders about opportunities to gain efficiencies. However, we often see leaders incorrectly use benchmark as a management tool. When this happens, we miss the opportunity to dig deeper to understand the opportunity and create a plan to improve. This can leave department leaders exasperated with chasing quarterly moving targets, but worse still, this approach can invite short sighted decisions that ultimately pose risks to patient care.
Read More
Issue #13: Is Your Department “Special”? Normalizations Matter.
If you’ve worked in healthcare operations leadership for more than 18 months, you have likely heard the term “Benchmark.” If you’ve led a department for more than 5 years, you’ve likely been on the wrong side of a benchmark comparison (or know a poor soul who has). This newsletter explores the data review required to ensure accurate submissions, ultimately supporting useful performance comparisons for all participants.
Read More
Issue #12: Are On-Call Schedule Demands Impacting Your Team's Engagement?
Traditional on-call programs impact department culture and finances. Call-back premium pay rates increase department labor expenses, and the demands of the call schedule can contribute to poor staff satisfaction, high turnover, and difficulty recruiting. In many cases, alternative solutions are more advantageous than the traditional on-call model.
Read More
Issue #11: Are You Using Contract Labor Effectively?
Contract labor resources are a true asset to healthcare organizations when utilized appropriately and managed well. However, many organizations find it challenging to align contract labor to their staffing needs while controlling overall labor expenses.
High performing organizations quantify anticipated needs for vacancies, leave of absence support, and seasonal workload volume fluctuations while ensuring contract labor is never used inappropriately through attentive management.
Read More
Issue #10: Pandemic Staffing: Our "New Normal"
Across the country, hospitals have been forced to close their doors due to revenue headwinds and increasing costs due to the COVID 19 pandemic. All are working to closely manage costs to keep their doors open for the communities they serve.
Perhaps the most approachable and impactful strategy to reduce cost while improving care is demand matching – the process of reviewing staff schedules and patient workload volumes to align staff with volume by hour of day. Even if you’ve done this in the past, it’s important to reevaluate as patient volume patterns have shifted in hospitals across the country.
Read More
Issue #9: Hiring Ahead of Turnover
Experienced leaders know the turnaround time for hiring and orienting staff creates a greater vacancy burden than is typically seen on paper. When staff are unavailable to work, we rely on premium labor such as overtime or travelers to care for our patients, which can adversely impact our culture, outcomes, and hospital finances.
Hiring ahead is a strategy that allows us to quantify the true vacancy burden and hire the perfect number of FTEs and reduce avoidable premium pay.
Read More
Issue #8: Zero Based Staffing Models
Productivity targets help hospitals balance resource requirements with financial goals by budgeting specific hours for the workload in each department. The process of setting productivity targets can present a challenge to both nursing and finance leaders as they work together to identify the ideal goal. By using zero based staffing models, industry leaders ensure that the right staff are in the right place at the right time.
Read More
Issue #7: Do You Manage Productivity Daily?
Top performing hospital leaders are always searching for innovative ways to reduce the cost of healthcare without adversely impacting care and services provided. Labor spend constitutes over half of total hospital expenses and is widely considered the most controllable expense. Daily productivity management can help hospitals reduce expenses without having to furlough or lay off staff members. A successful strategy includes two primary components: increased performance visibility through daily reporting and managing improvement through department action plans to remedy missed targets.
Read More
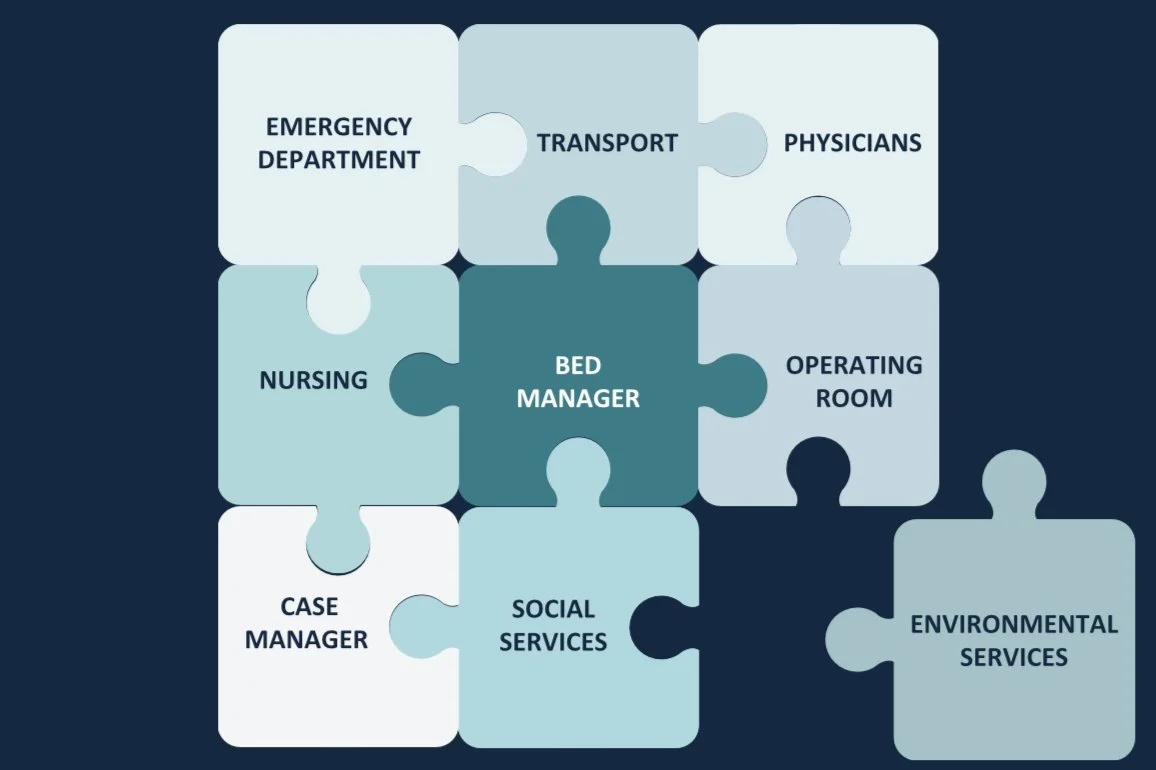
Issue #6: 10 Best Practices to Manage Hospital Capacity
Hospitals across the country are faced with daily bed management challenges. With ED admissions typically peaking between 3:00pm to 7:00pm, PACU admissions between 12:00pm to 4:00pm, and inpatient discharges between 6:00pm to 8:00pm, it is easy to see why capacity challenges exist. Now, more than ever, capacity management requires thoughtful consideration to maximize appropriate utilization of beds, staff, and services. CCC team member, Susie Law shares key tactics for maximizing hospital capacity in this article.
Read More
Issue #5: Are Your Expenses Outpacing Your Revenue Due to COVID-19?
Revenue degradation experienced due to the COVID-19 pandemic is impacting hospital finances across the country. Suspension of elective surgeries and procedures threatens the viability of many healthcare organizations. After decades of experience in the for-profit sector, our team has summarized some of the top impact expense management strategies. Continue reading for a high level view and check out our article for more details.
Read More