THANK YOU FOR SUBSCRIBING!!!
Nursing shortages and vacancies have always been an issue in healthcare operations, but every year it is becoming more concerning, and even crippling, in hospitals across the country.
Unfortunately, there is no one-size-fits-all solution when it comes to staffing shortages. However, there are proven best practices that can make a difference!
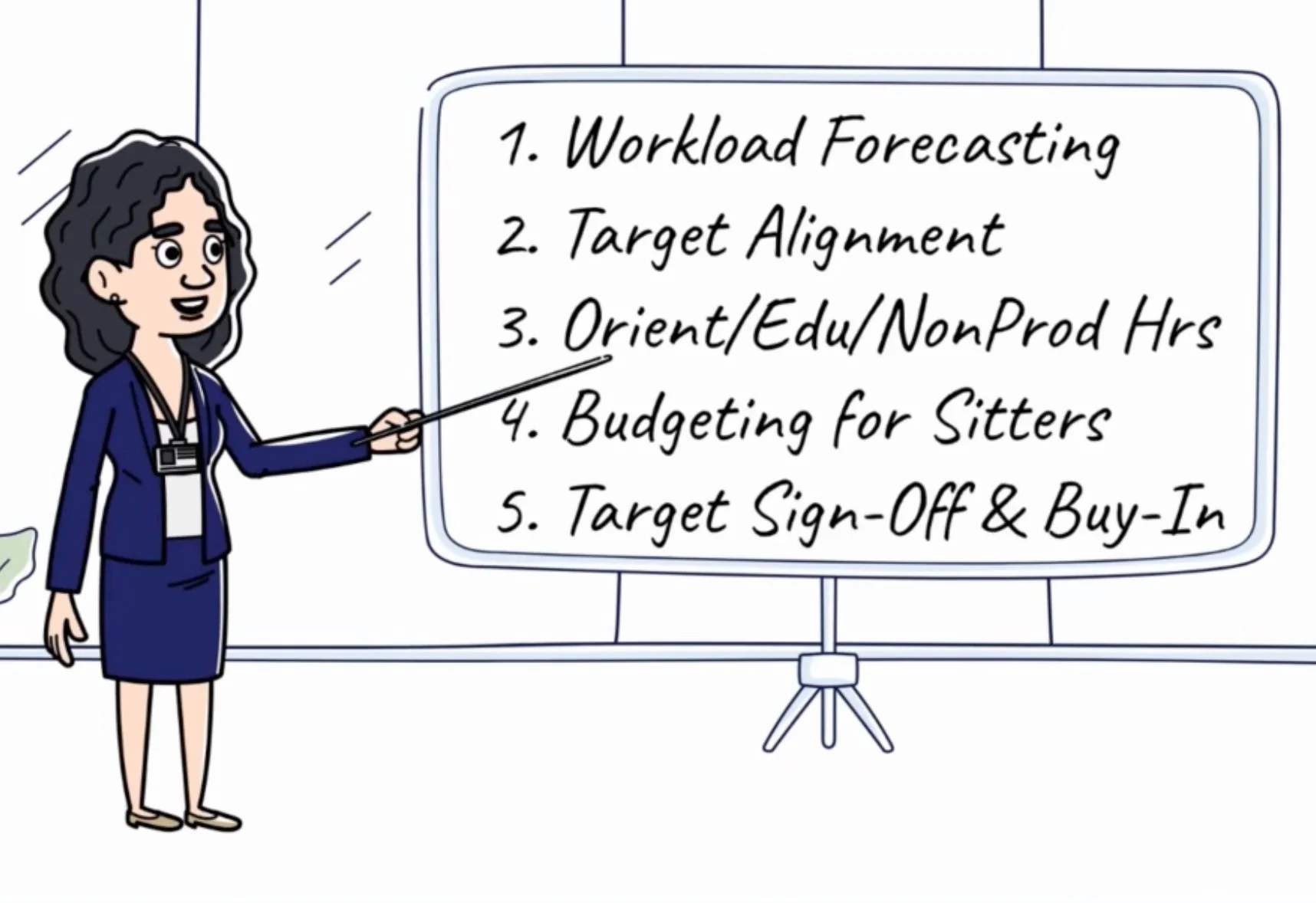
Uninformed labor cost projections can make or break your budget, but it can be tough to know where to start - which is why we've prioritized 5 key areas of focus for you! If you're looking for a hospital FTE budget study guide, keeping reading!
Have you ever wondered how finance sets a department's budget each year? While most explanations we've heard sound quite complex, the truth is quite simple.
There are only 3 ways to set a productivity target: Run Rate, Benchmark, and Zero-Base
Leaders struggling with their target often ask this question and most are unable to get a straight answer - perhaps because the person they are asking isn't sure. This common complaint inspired us to share this newsletter and we hope it helps!
How do organizations accurately determine the number of Full-Time Equivalents (FTEs) needed to fill staff schedules without requiring overtime?
If you’ve ever worked on this problem, you know that hiring 30 FTEs does NOT imply 30 FTEs will be worked. This means FTE totals taken from the HRIS system are unreliable (no, we aren’t referencing nonproductive time, although it also must be considered when calculating productive availability)!
To truly understand staffing commitment, we must review historically worked hours for each team member. A team member’s commitment is defined as the weekly hours they have agreed to work. As an example, 0.9 FTE RNs are hired to work 36 hours per week (typically in a 3x12 shift format).
Analyzing FTE availability begins with comparing this agreed-upon FTE commitment with actual worked hours.
How confident are you that your managers and directors are prepared to lead their teams?
Are you sure they have the tools they need to do a great job?
If so, you’re ahead of most. In healthcare we have SO many opportunities to improve, but we commonly trip over the finish line when it comes to execution. When it comes to change management, accountability is key, but support is often overlooked.
We observe poor leadership preparedness all the time – seeing it everywhere from academic medical centers to community hospitals – so we designed a solution– or at least part of one. Whether it is information about industry best practices or simply supporting sustainable growth through 1:1 coaching a resource to support improvement for new and tenured leaders should be available to them.
Both support and accountability are required to drive results, so understanding your role in this respect is critically important.
Support includes activities like education, 1:1 time, tools, communication, setting expectations, and other activities that help individuals achieve their goals. Accountability, on the other hand, facilitates individual responsibility including leveraging reports to ask tough questions, ensuring deadlines are met and that rules are enforced.
In the education field, our job is almost 100% support. What about yours?
Staffing grids connect clinical and financial guidelines in a way that effectively supports sustainable operations.
We aren't sure how long they've been around, but we would assume that the first staffing grid is older than anyone reading this, given how beautifully simple and impactful these little pieces of paper can be.
Does your nursing unit's staffing grid align with the budget financially? Are your nursing units staffing in alignment with their grids? How do you know? How do you ensure consistent nursing ratios between units? Across multiple hospitals in a health system?
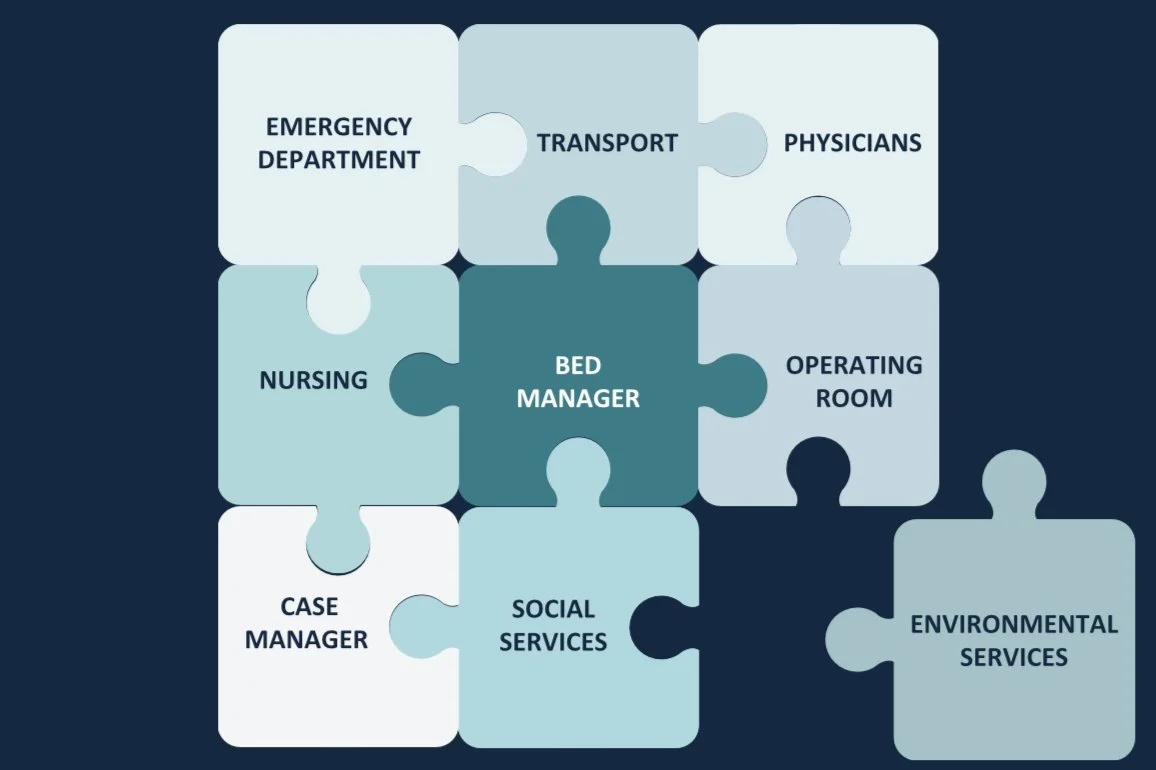
Is the ER solely responsible for boarders at your hospital? If so, #youredoingitwrong!
While patients with admission orders waiting to go upstairs are physically in the ER, the drivers of their delay has very little to do with the ER itself. The truth about boarders is that they are primarily driven by inefficient processes on the inpatient side, while the ER pays the price.
According to the CDC, more than 1.5 million would-be ER patients leave without being seen each year in the US. Exacerbated by the pandemic, the Left Without Being Seen (LWBS) rate has skyrocketed, leading to significant lost revenue for hospitals who desperately need it to support staffing levels. Ensuring patients receive care when they need it is a critical part of supporting the communities we serve. Design a plan to keep both patients and finances healthy with proven ER best practices.
Many organizations implement float pools to help cover unexpected gaps in schedules, but without a thoughtful approach and proper planning, they routinely fail – sometimes costing their organizations millions per month in avoidable spend with no end in sight.
Departments request float pool resources for all open shifts, regardless of the reason. However, successful labor leaders understand that each type of resource demand - due to vacancy, maternity leave, seasonal peak volumes, etc - requires a specific support strategy.